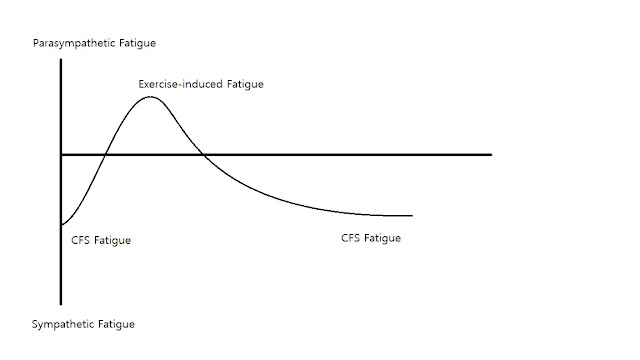
Since I got Polar H7, I decided to look into the heart rate variability (HRV) and see if it has any correlation to fatigue. I only got 2 weeks worth of data so far, so I can't write it up yet. I'll do that when I have at least 1 month's worth of data. But the topic of sympathetic and anti-sympathetic fatigue popped in the process of looking into it. Various exercise training sites and HRV apps claim that low HRV correlates to stress/deconditioning while the high value corresponds to exercise-induced fatigue.
According to this theory, the stress/deconditioning fatigue requires active recovery (exercise) while exercise-induced fatigue requires rest to recover from it. Sympathetic nerve dominates during the former and HRV plummets. Conversely, Parasympathetic nerve takes over during the latter and HRV goes up. When I came across an article about
sympathetic vs parasympathetic overtraining syndrome years ago while researching OTS, I didn't quite understand it. Now they all fit together, at least in theory.
Healthy individuals experience fatigue when deconditioned or mentally stressed. This fatigue is alleviated by exercise. The body goes into parasympathetic dominated mode while trying to recover from exercise and the CNS balance is restored with the rest:
 |
| 1 - Normal Fatigue Curve |
CFS patients, on the other hand, don't get such relief. They are perennially in sympathetic fatigue state and they cannot exercise enough to produce exercise-induced fatigue because they reach the post-exertional sickness threshold of CFS well before they can reach the exercise threshold. Therefore the exercise triggers post-exertional sickness instead, making the CFS fatigue worse:
 |
| 2 - CFS Fatigue Curve |
Competitive athletes reaches their exercise limit first. If they continue to push without adequate recovery, however, they can reach the over-training threshold and end up with OTS fatigue:
 |
| 3- OTS Fatigue Curve |
Notice the similarity of this curve to the CFS fatigue curve. The difference is that, in case of OTS, the over-training threshold is above the exercise limit while the post-exertional sickness threshold for CFS is below the exercise limit. Post-exertional sickness can be viewed as the overtraining syndrome for CFS patients in this sense, except that it gets triggered much easier because its threshold is well below the exercise limit.
Until recently, my fatigue followed the CFS fatigue curve. I'd keel over whenever I walk more than 2km or walk just a little bit faster. But that has changed for some reason since July. Now I can walk 2 miles without getting sick. The morning after the walk, I am getting the
post-exercise fatigue that I recover from rather than plunging into post-exertional sickness. The graph now looks like this:
These fatigue curves are all theory of course, and I haven't seen any data to prove it. I'll write up some more when I have enough HRV data. Even if my data confirms, it is a trial with only one patient for 30 or so observations. And obviously no randomization or blinding either. In other words, it still is no more than an anecdote. But it seems like a nice model to visualize CFS vs normal fatigue, regardless.